The Relationship Between Obesity, PCOS, and Menopause in Women
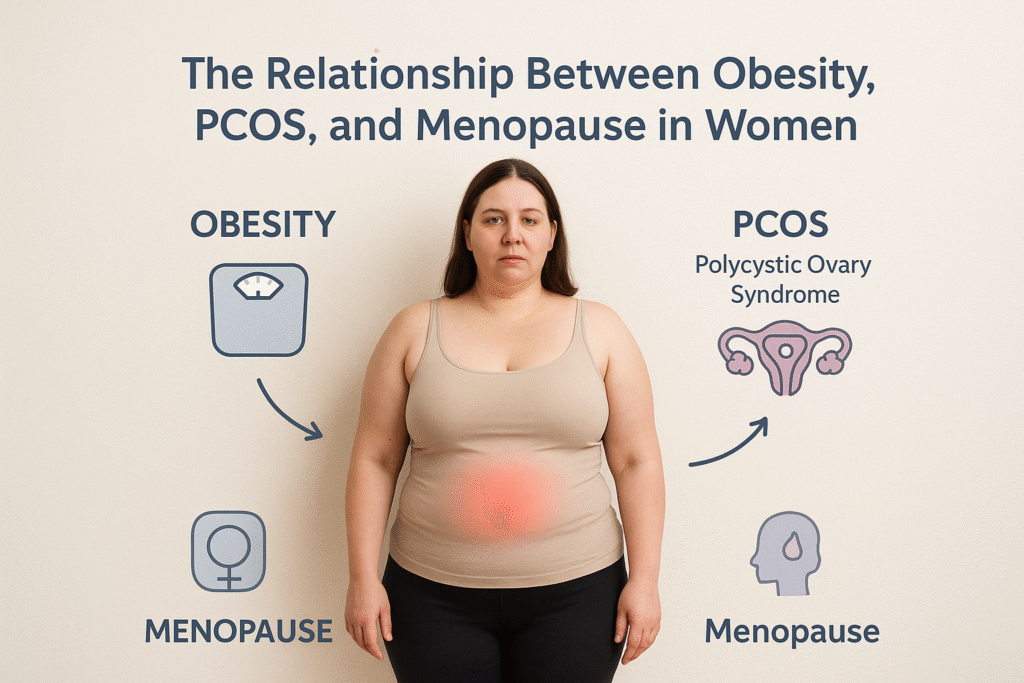
BMI Calculator +91 9820062040 | +91 8356977265 enquiry@thedigestive.in Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations The Relationship Between Obesity, PCOS, and Menopause in Women Women’s health is shaped by a complex interplay of hormones, metabolism, and life-stage transitions. Two conditions that stand out for their significant impact on women are Polycystic Ovary Syndrome (PCOS) and menopause. While both are distinct phases of reproductive and metabolic health, obesity often acts as a connecting factor, influencing the onset, severity, and outcomes of each. In this three-part series, we’ll explore how obesity, PCOS, and menopause are interlinked, why women face heightened risks at different stages of life, and what strategies exist for prevention and management. Understanding Obesity in Women’s Health Obesity is defined by the World Health Organization (WHO) as abnormal or excessive fat accumulation that may impair health. A Body Mass Index (BMI) of 30 or above indicates obesity. But in women, obesity does more than increase risk for cardiovascular diseases or diabetes—it disrupts reproductive health. – Why Women Are at Greater Risk Hormonal fluctuations: Estrogen, progesterone, and androgens influence fat storage and metabolism. Life-stage transitions: Puberty, pregnancy, perimenopause, and menopause all increase vulnerability to weight gain. Metabolic differences: Women naturally have higher body fat percentages than men, making weight management biologically harder. – The Vicious Cycle Obesity triggers insulin resistance and chronic inflammation, which worsen hormonal imbalances. In turn, these hormonal disruptions promote fat storage—creating a cycle that’s difficult to break. What Is Polycystic Ovary Syndrome (PCOS)? PCOS is a common endocrine disorder affecting 1 in 10 women of reproductive age worldwide. It is characterized by: Irregular or absent periods Excess androgen levels (leading to acne, hirsutism, hair thinning) Polycystic ovaries visible on ultrasound – The Role of Obesity in PCOS Obesity is not the cause of PCOS, but it worsens the condition. Around 40–80% of women with PCOS are overweight or obese. Excess fat, particularly visceral fat around the abdomen, aggravates insulin resistance, which in turn drives androgen production. This results in: More severe menstrual irregularities Higher risk of infertility Greater metabolic complications (prediabetes, diabetes, heart disease) – Insulin Resistance as a Common Link Both obesity and PCOS share insulin resistance as
Top 10 Common Causes of Obesity You Should Know

BMI Calculator +91 9820062040 | +91 8356977265 enquiry@thedigestive.in Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Top 10 Common Causes of Obesity You Should Know Obesity is no longer just a cosmetic concern—it has become one of the most significant global health challenges of the 21st century. According to the World Health Organization (WHO), worldwide obesity rates have nearly tripled since 1975. Today, more than 1 billion people are obese, including 650 million adults, 340 million adolescents, and 39 million children. These numbers continue to rise at an alarming rate. While genetics and environment play a role, most obesity cases are preventable. Understanding the causes of obesity can help you make informed lifestyle choices, improve your health, and even reduce your risk of chronic diseases such as diabetes, heart disease, hypertension, and certain cancers. In this article, we’ll explore the top 10 most common causes of obesity, along with practical prevention strategies, weight loss tips, and treatment options—including bariatric surgery for severe cases. Let’s dive deeper into the root causes and find out how to overcome them. 1. Poor Dietary Habits One of the most obvious yet most overlooked causes of obesity is an unhealthy diet. Modern food culture encourages consumption of calorie-dense, nutrient-poor foods that contribute directly to weight gain. Foods and eating patterns that promote obesity: Fast food and fried items: Burgers, fries, and pizzas are packed with unhealthy fats and refined carbs. Sugary drinks: Sodas, energy drinks, and packaged juices often contain more sugar than a dessert. Processed snacks: Chips, biscuits, instant noodles, and packaged sweets provide empty calories. Large portion sizes: Supersized meals condition people to eat more than their body needs. Over time, these habits cause a calorie surplus, leading to fat storage, especially around the abdomen. Weight loss tips for diet improvement: Replace refined carbohydrates with whole grains such as oats, quinoa, and brown rice. Cut down on added sugars by avoiding packaged drinks and opting for water or unsweetened teas. Cook more meals at home to control ingredients and portion sizes. Follow the 80/20 rule: Eat nutrient-rich foods 80% of the time, and allow indulgence 20% of the time. A healthy diet isn’t about strict restrictions—it’s
Walking for Weight Loss: How Many Steps Do You Need Daily?

BMI Calculator +91 9820062040 | +91 8356977265 enquiry@thedigestive.in Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Walking for Weight Loss: How Many Steps Do You Need Daily? Walking as a Sustainable Weight Loss Tool Walking is one of the most natural and accessible forms of physical activity for adults and older teens. Unlike high-intensity workouts or medical interventions such as bariatric surgery, walking is low-impact, safe, and can be incorporated into daily routines without special equipment. Evidence shows that regular walking contributes significantly to weight loss, fat reduction, and obesity management. According to the Centers for Disease Control and Prevention (CDC), adults should aim for at least 150 minutes of moderate-intensity physical activity per week, and walking is a practical way to achieve this goal. The question many people ask is: How many steps per day are needed to see meaningful weight loss? The answer varies depending on factors such as body weight, age, metabolic rate, and diet. This blog provides evidence-based guidance on step goals, walking intensity, and practical tips for long-term weight management. How Walking Supports Weight Loss Walking helps in multiple ways: Burns Calories: Walking increases total energy expenditure, creating a caloric deficit that is essential for weight loss. Boosts Metabolism: Brisk walking can elevate heart rate and stimulate fat metabolism, particularly when done consistently. Low Risk of Injury: Walking is gentle on the joints and suitable for overweight or obese individuals. Reduces Stress: Walking reduces cortisol levels, preventing stress-induced fat storage around the abdomen. Improves Overall Health: Beyond weight loss, walking lowers the risk of cardiovascular disease, diabetes, and high blood pressure. A study published in the Journal of Physical Activity & Health found that walking 10,000 steps per day is associated with improved body composition and decreased waist circumference in adults. Walking vs Other Weight Loss Methods Method Pros Cons Walking Low-impact, sustainable, improves cardiovascular health Slower calorie burn than high-intensity exercise Running Burns more calories per minute, quick results Harder on joints, may be challenging for overweight individuals Gym Workouts Builds strength and tone muscles Requires time, money, and motivation Bariatric Surgery Rapid weight loss for severe obesity Invasive, costly, long-term dietary restrictions Walking may not offer
Post-pregnancy Weight Loss: Safe and Effective Tips for New Mothers

BMI Calculator +91 9820062040 | +91 8356977265 enquiry@thedigestive.in Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Post-pregnancy Weight Loss: Safe and Effective Tips for New Mothers Bringing a baby into the world is a beautiful experience, but for many mothers, the journey doesn’t end with childbirth. The postpartum period comes with physical, emotional, and lifestyle changes. One of the most common challenges new mothers face is post pregnancy weight gain. While it’s natural to gain weight during pregnancy, many women struggle to shed those extra kilos after delivery. If not managed carefully, weight issues after childbirth can lead to long-term health risks such as obesity, diabetes, and even postpartum depression. The good news is that with the right strategies, postpartum weight loss can be both safe and effective. This article dives deep into the causes of post-pregnancy weight gain, science-backed weight loss methods, lifestyle adjustments, and tips to ensure new mothers prioritize health without compromising their recovery. Why Post Pregnancy Weight Gain Happens Every woman’s body responds differently to pregnancy, but some common causes of postpartum weight gain include: Hormonal changes: Fluctuations in estrogen and progesterone can slow metabolism. Increased calorie intake during pregnancy: Many women continue pregnancy eating habits after delivery. Sedentary lifestyle: Recovery period reduces activity levels. Sleep deprivation: Lack of sleep increases cravings and stress hormones. Emotional eating: Stress, fatigue, and postpartum depression may trigger overeating. Understanding these factors is the first step toward achieving healthy postpartum weight loss. Postpartum Recovery: Why Weight Loss Should Be Gradual It’s important to remember that weight loss after childbirth is not about quick fixes. Doctors recommend waiting 6–8 weeks after delivery before starting any active weight loss plan. For mothers who have undergone C-section, recovery may take longer. Why gradual weight loss is essential: Prevents nutrient deficiency while breastfeeding. Allows the body to heal internally. Reduces the risk of postpartum depression triggered by extreme dieting. Helps build sustainable habits for long-term weight management. The goal should be health and well-being, not just numbers on the scale. Safe Postpartum Weight Loss Tips for New Mothers 1. Focus on Balanced Nutrition Your diet plays the biggest role in postpartum recovery and weight management. Eat whole
Childhood Obesity in India: Why It’s Rising and How to Control It
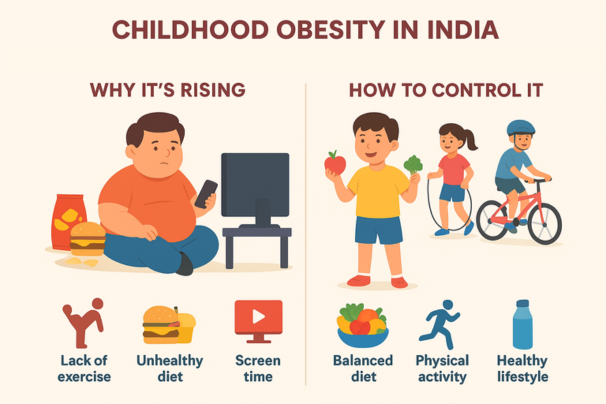
BMI Calculator +91 9820062040 | +91 8356977265 enquiry@thedigestive.in Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Childhood Obesity in India: Why It’s Rising and How to Control It Childhood obesity is emerging as one of India’s most pressing public health challenges. Once seen primarily in developed countries, it is now spreading rapidly across urban and even semi-urban India. According to the Indian Journal of Community Medicine, nearly 14.4 million children in India are obese, making it the second-largest country in terms of childhood obesity cases. Understanding the causes of obesity in children is crucial to reversing this trend. From poor diets and sedentary lifestyles to socioeconomic changes and lack of awareness, multiple factors are fueling the epidemic. If left unchecked, childhood obesity can lead to early onset of diabetes, heart disease, and lifelong health struggles. In this detailed blog, we’ll explore: Why childhood obesity in India is on the rise The key causes of obesity in children Long-term risks and complications Effective weight loss tips and obesity treatment options How families, schools, and healthcare providers can work together Let’s break down this growing crisis and see how it can be controlled. Why Childhood Obesity Is Rising in India Childhood obesity in India is increasing at an alarming rate, with both urbanization and lifestyle modernization playing major roles. Key factors behind the rise: Urban lifestyles: Children in cities have easy access to fast food and limited open spaces for physical activity. Dietary shifts: Traditional home-cooked meals are being replaced by processed foods and sugary drinks. Technology dependence: Screen time has increased dramatically, reducing outdoor play. Socioeconomic growth: With rising income levels, families are spending more on calorie-dense foods. In short, modernization has improved convenience but has also created an environment where children are more likely to consume excess calories and move less—two of the primary causes of obesity. Top Causes of Obesity in Indian Children To address the problem effectively, we must identify the root causes of obesity among children. 1. Unhealthy Dietary Habits The most direct cause is poor diet. Junk food is easily available, heavily marketed, and often considered “cool” by children. Processed snacks like chips, instant noodles, and biscuits dominate school
Obesity and Its Impact: How Bariatric Surgery Can Help Reverse Chronic Diseases
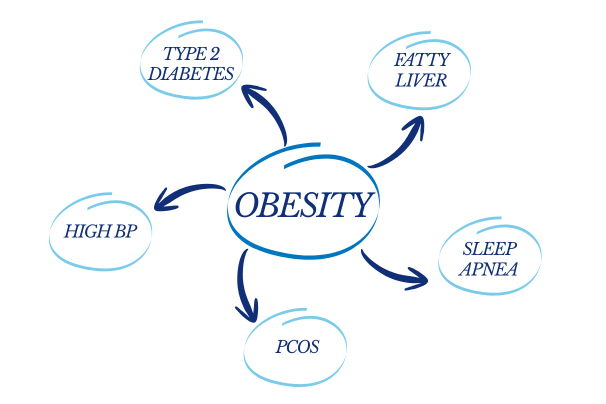
BMI Calculator +91 9820062040 | +91 8356977265 enquiry@thedigestive.in Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Obesity and Its Impact: How Bariatric Surgery Can Help Reverse Chronic Diseases Obesity is more than just a number on the weighing scale. It is a complex, chronic health condition that affects nearly every organ system in the body. Today, rising obesity rates are directly linked to the increased prevalence of life-altering diseases such as Type 2 diabetes, hypertension, PCOS, sleep apnea, and fatty liver disease. But there is hope. For those struggling with severe obesity and its related complications, bariatric surgery offers a powerful, scientifically backed intervention — not just for weight loss, but for reversing these chronic conditions. In this blog, we explore how obesity impacts the body, how these conditions are interconnected, and how procedures offered at the Digestive Health Institute by Dr. Muffi can help transform lives. 1. The Growing Burden of Obesity According to the World Health Organization (WHO), obesity has tripled worldwide since 1975. In India, more than 135 million people are affected by overweight and obesity — and the numbers are steadily rising. Obesity is not merely a cosmetic issue. It increases the risk of developing over 50 different health conditions. Even more concerning, it shortens life expectancy and impacts physical, emotional, and social well-being. 2. Diseases Linked to Obesity – Type 2 Diabetes Excess fat, especially abdominal fat, causes insulin resistance — where the body fails to respond to insulin properly. This leads to elevated blood sugar levels and ultimately results in Type 2 Diabetes. According to the International Diabetes Federation, more than 80% of people with Type 2 diabetes are overweight or obese. – Hypertension (High Blood Pressure) Obesity increases the workload on the heart. The excess fat tissue needs more oxygen and nutrients, which causes the heart to pump harder. This additional effort raises blood pressure levels, leading to chronic hypertension — a silent killer that significantly increases the risk of heart attacks and strokes. – PCOS (Polycystic Ovary Syndrome) In women, obesity aggravates hormonal imbalances and insulin resistance, both of which are key drivers of PCOS. Obese women with PCOS often experience irregular menstrual cycles, infertility,
Thirst vs Hunger: How Dehydration Leads to Overeating
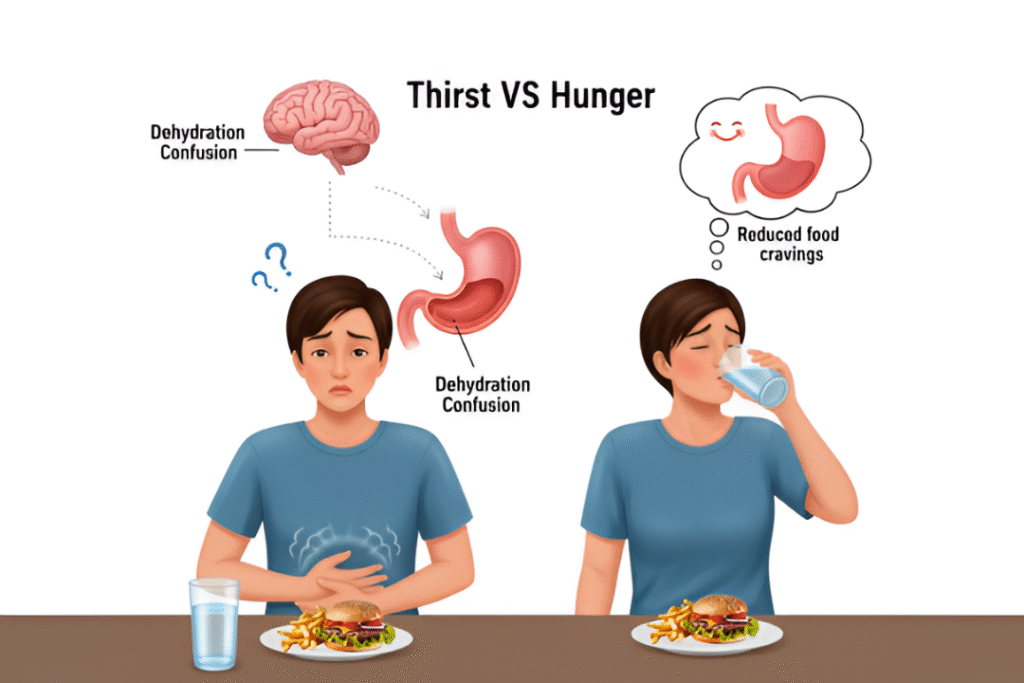
BMI Calculator +91 9820062040 | +91 8356977265 enquiry@thedigestive.in Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Thirst vs Hunger: How Dehydration Leads to Overeating Thirst vs. Hunger – A Costly Confusion Many people start their health journey focusing on calories, carbs, and workout routines — but forget to check something much more basic: hydration. Believe it or not, a simple glass of water might be the key to unlocking your weight loss potential. Confusing thirst for hunger is a common mistake that can lead to unnecessary snacking, excess calorie intake, and ultimately — obesity. This confusion is more than a bad habit; it’s a physiological trap that even the most health-conscious individuals can fall into. In this blog, we’ll explore: Why dehydration is often mistaken for hunger How this leads to weight gain The science behind hydration and metabolism The benefits of protein water (like Soulfuel Orange) Why this matters before and after bariatric surgery Let’s dive in. The Science: Why We Mistake Thirst for Hunger Your body’s thirst and hunger signals are both controlled by a part of the brain called the hypothalamus. When you’re even mildly dehydrated, the hypothalamus can misinterpret thirst cues as hunger, making you reach for a snack when what your body really needs is fluids. – What Happens When You’re Dehydrated: Your body craves something to replenish energy → food is the easiest go-to. Brain fog and irritability rise → leading to emotional eating. Your mouth feels dry → and chewing sounds like a fix, so you eat. You feel tired → but instead of drinking water, you reach for sugar-laden snacks or caffeine. This chain reaction creates a caloric surplus over time, leading to weight gain and even obesity — especially when combined with a sedentary lifestyle. Dehydration and Obesity: The Hidden Connection The relationship between dehydration and obesity isn’t just anecdotal. Research has shown that: People who are well-hydrated have better control over their appetite. Mild dehydration can reduce cognitive performance, leading to emotional eating. Irritability and stress eating increase when the body is dehydrated. – A Dangerous Cycle: You feel hungry — but it’s thirst. You snack unnecessarily. You gain weight. Obesity increases your
The Role of High-Fiber Foods in Managing Hunger and Preventing Overeating
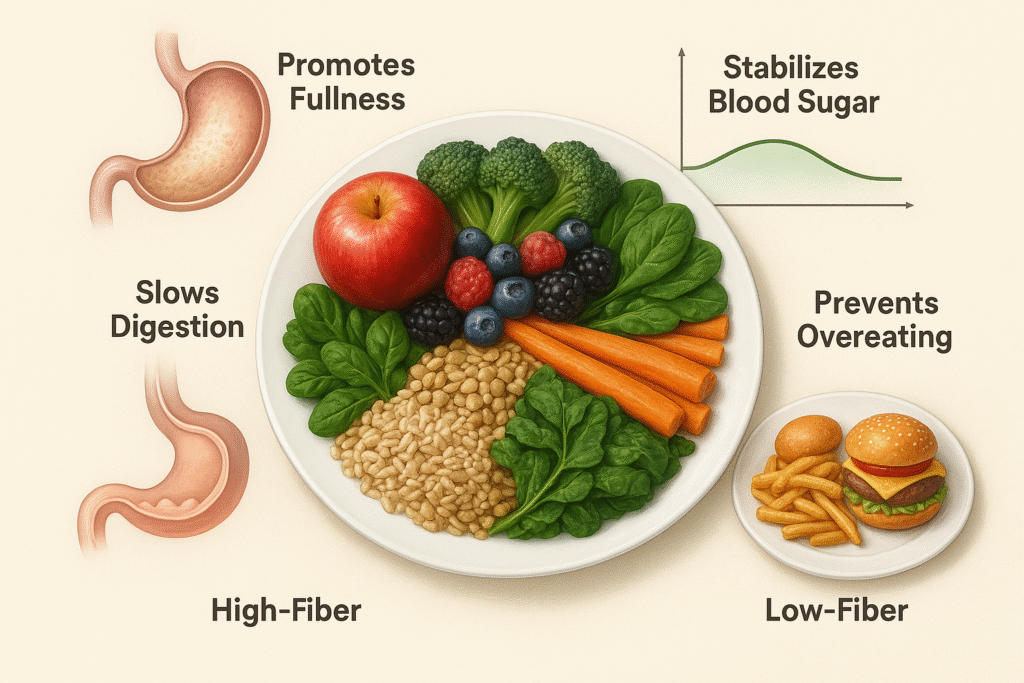
BMI Calculator +91 9820062040 | +91 8356977265 enquiry@thedigestive.in Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations The Role of High-Fiber Foods in Managing Hunger and Preventing Overeating In the age of fast food, fad diets, and ultra-processed meals, one simple yet powerful dietary component often gets overlooked—fiber. While it’s not glamorous or trending on social media, fiber plays a crucial role in managing hunger, promoting satiety, and preventing overeating. For individuals trying to lose weight, regulate blood sugar, or simply eat more mindfully, increasing dietary fiber can be a sustainable strategy. This blog dives deep into the science, benefits, and practical ways to integrate high-fiber foods into everyday meals. What is Dietary Fiber? Dietary fiber is a type of carbohydrate found in plant-based foods. Unlike other carbs, fiber isn’t digested or absorbed by the body. Instead, it passes relatively intact through your stomach, small intestine, and colon. – Types of Fiber Soluble Fiber – Dissolves in water to form a gel-like substance. Helps slow digestion and is excellent for blood sugar control. Found in: Oats, legumes, apples, berries, carrots, citrus fruits. Insoluble Fiber – Adds bulk to stool and helps food pass more quickly through the stomach and intestines. Found in: Whole grains, wheat bran, nuts, seeds, and vegetables like cauliflower and green beans. How Fiber Helps Manage Hunger – Slows Down Digestion Soluble fiber forms a viscous gel in the gut, which slows the digestion of food and the absorption of nutrients. This leads to a prolonged feeling of fullness, reducing the urge to eat frequently. – Reduces Appetite Hormones Several studies show that a high-fiber meal can reduce levels of ghrelin, the hormone that signals hunger to the brain, and increase peptide YY and GLP-1, which signal satiety. – Increases Chewing Time High-fiber foods often require more chewing, which can: Promote mindfulness during eating Allow time for satiety signals to reach the brain Reduce the likelihood of overeating – Adds Volume Without Calories Fiber-rich foods are generally lower in energy density (calories per gram). You can eat larger volumes without consuming too many calories. Scientific Evidence Supporting Fiber’s Role in Satiety – Clinical Studies In dietary counseling, patients
Why Do People Regain Weight After Weight Loss Surgery?

BMI Calculator +91 9820062040 | +91 8356977265 enquiry@thedigestive.in Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Why Do People Regain Weight After Weight Loss Surgery? Weight loss surgery, also known as bariatric surgery, has helped thousands achieve healthier lives, especially when traditional methods like dieting and exercise fall short. However, many people are surprised to learn that some weight regain is not uncommon after a few years. This doesn’t mean surgery has failed—it just means that long-term success depends on lifestyle, support, and understanding the changes the body goes through. In this blog, we’ll explore the real reasons why some people regain weight after surgery—and more importantly, how to prevent it. If you’re considering or recovering from weight loss surgery, this guide will help you set realistic expectations and stay on track. 1. Understanding How Weight Loss Surgery Works Before exploring the reasons behind post-surgical weight regain, it’s essential to understand how bariatric surgery actually facilitates weight loss. There are several types of surgeries, including: Roux-en-Y Gastric Bypass (RYGB): Reduces stomach size and bypasses part of the small intestine. Sleeve Gastrectomy (VSG): Removes a large portion of the stomach, creating a “sleeve” shape. Mini-Gastric Bypass (MGB): Similar to RYGB but with a simplified design. Adjustable Gastric Banding (Lap-Band): Uses a band to restrict stomach size. These surgeries reduce the stomach’s capacity, lower calorie absorption, and affect gut hormones like ghrelin, which suppress hunger. Patients typically experience significant weight loss within the first year, often accompanied by better control over comorbidities like high blood pressure and sleep apnea.But surgery is only the beginning of a lifelong journey. 2. How Common Is Weight Regain After Bariatric Surgery? It’s important to normalize the conversation around weight regain—it’s not uncommon. Studies indicate: 30–50% of patients regain some or most of the lost weight within 2–5 years after surgery. 10–20% of patients may regain nearly all the weight they initially lost. It’s not always a full reversal, but the partial gain is enough to bring back obesity-related health concerns, impact mental well-being, and undo years of progress if not addressed. 3. Top Reasons Why People Regain Weight Post-Surgery -Stretching of the Stomach Pouch After procedures like sleeve gastrectomy
What is Robotic surgery?
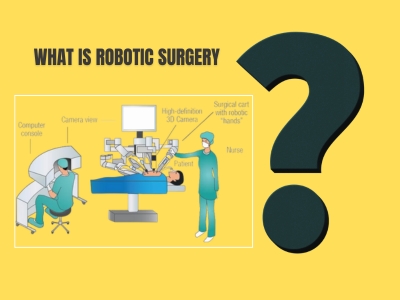
BMI Calculator +91 9820062040 | +91 8356977265 enquiry@thedigestive.in Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala, Founder Our Team Outreach OPD Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S Obesity Surgery Endoscopic-Gastric Balloon Endoscopic-Gastric Sleeve Revisional Bariatric Surgery Roux En Y Gastric Bypass SADI (malabsorptive) Sleeve Gastrectomy Sleeve + Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition General Surgery General Surgery Adrenalectomy (Adrenal gland Removal) Appendectomy (Appendix Surgery) Cholecystectomy (Gallbladder Surgery) Hernia Surgery Hysterectomy (Uterus Removal Surgery) Splenectomy (Spleen Removal) VATS (Video-Assisted Thoracoscopy – Key hole Chest Surgery) GI Surgery Hydatid Cyst Removal (Liver Cyst Removal) Puestow’s Procedure (Chronic Pancreatitis Drainage Surgery) GI Oncology Gastric (Stomach) Cancer GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer (Colon & Rectum) Small Intestine Cancer (Small Bowel) Whipple’s Surgery (Pancreatic Cancer) Media & Stories Testimonials Our Health Partners Press Blogs Journal & Publication Connect Contact Us Locations Digestive Health Institute by Dr. Muffi Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations Home About us Dr. Muffazal Lakdawala Our Team Outreach OPD’s Training & Workshops Science & Magic of DHI Global Patient Program Work with DHI Eat Right Prescription Weight Management Optimal Weight Child Nutrition Lifestyle Nutrition Weight Management Gut Care Gut Reset Expert Care Diabetes Control Menopause Wellness PCOS Management Post Surgery Nutrition Obesity surgery Endoscopic- Gastric Balloon Endoscopic- Gastric Sleeve Revisional Bariatric Surgeries Roux En Y Gastric Bypass SADI Procedure Sleeve Gastrectomy Sleeve + Support Emotional Wellness Rehabilitation Therapy Restorative Plastic Surgery Nutritional Supplements Obesity Support Group Test & Investigations Common FAQ’S General Surgery General Surgery Adrenalectomy Appendectomy Cholecystectomy Hernia Surgery Hysterectomy Splenectomy Video-Assissted Thoracoscopy (VATS) GI Surgery Hydatid Cyst Removal Puestow’s Procedure GI Oncology Stomach Cancers GEJ (Gastroesophageal Junction) Cancer Large Intestine Cancer Small Intestine Cancer Whipple’s Surgery Media & Stories Testimonials Our Partners Press Blogs Journal & Publications Connect Contact Us Locations What is Robotic Surgery ? Surgical care has evolved dramatically over the past century—from the era of large, invasive incisions and prolonged hospital stays to today’s highly advanced, minimally invasive procedures. What once required open surgery with significant recovery time can now be accomplished through keyhole incisions with unmatched precision, thanks to the advent of robotic-assisted surgery. In the early days, surgery was often seen as a last resort. The tools were basic, the procedures were lengthy, and outcomes carried considerable risk. The introduction of laparoscopic surgery in the late 20th century marked a major breakthrough. It allowed surgeons to operate using small incisions, guided by cameras and long instruments. This approach reduced pain, minimized complications, and helped patients recover faster. However, even laparoscopy had its limitations—restricted range of motion, reduced visibility, and physical strain on surgeons during long operations. The next leap forward came with the development of robotic surgical systems—a technological evolution that has redefined what modern surgery can achieve. These systems combine a surgeon’s expertise with the precision of robotic arms, offering three-dimensional high-definition views and a level of control that exceeds the human hand. Robotic surgery enhances safety, accuracy, and outcomes, especially in complex procedures involving the digestive system and internal organs. What is Robotic Surgery? Robotic surgery is a cutting-edge surgical technique that uses computer-assisted robotic systems to perform complex procedures with enhanced precision, flexibility, and control. Unlike traditional open surgery, where a surgeon operates directly with their hands, or even standard laparoscopy which relies on rigid instruments, robotic surgery allows the surgeon to operate from a specialized console, where every movement of their hands is translated into real-time, fine-tuned actions by robotic arms inside the patient’s body. The most well-known system used globally is the da Vinci Surgical System, which has transformed the landscape of minimally invasive surgery. This system comprises three main components: Surgeon Console: Here, the surgeon sits comfortably and views the surgical site in high-definition 3D, magnified up to 10 times. Using master controls and foot pedals, the surgeon manipulates the robotic arms with precision. Patient-side Robotic Arms: These robotic arms are attached to tiny